One of the less invasive methods of remedying persistent discomfort from protruding spinal disc material is percutaneous (“through the skin”) disc decompression. Also referred to as nucleoplasty, it’s a procedure first developed in the 1960s. The latest version of the technique involves the use of plasma technology. Performed while the patient is awake, the alternative to traditional open surgery involves the insertion of a special transmitter into the disc to reduce tissue volume and stop nerve irritation.
How It’s Done
Normally taking about 20 to 30 minutes to perform, a percutaneous disc decompression requires light sedation and the application of a topical anesthetic to ease discomfort. As the patient remains awake, a micro-engineered alloy transmitter is placed inside of the disc that’s causing a patient’s pain. A special camera (fluoroscope) guides the doctor to the correct location. Some forms of the procedure are performed through a needle or catheter.
What It Means for Patients
Radio wave signals delivered to the inserted transmitter produce ionized gas. This low-temperature gas gently breaks molecular bonds in the center of the disc. The result is a less bulky disc, which reduces the overall size of the disc. For patients, it often means relief from radiating nerve pain when the nerve root is no longer irritated by the disc. Many patients also benefit from:
- Same-day relief of painful symptoms
- A faster return to normal activities
- Very few risks or potential side effects
Who’s Likely to Benefit
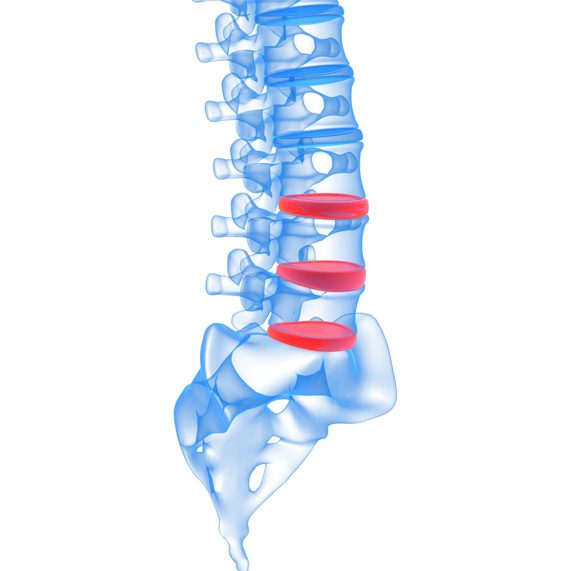
Percutaneous disc decompression is typically an option when discomfort is linked to a smaller herniated disc. Ideal candidates for the procedure are ones who do not have other possible sources for their pain. It’s not recommended as a treatment for pain related to spinal stenosis. Image tests and other diagnostic evaluations are often used to positively determine whether or not a patient’s pain is primarily from a herniated disc. It may also benefit patients with larger herniations that haven’t ruptured since traditional open surgery usually isn’t an option for situations like this.
Recovery and Long-Term Results
Patients frequently enjoy a much faster recovery time than what’s experienced with traditional decompression surgery along with fewer instances of symptoms returning. Strenuous exercise and heavy lifting should be avoided for a few weeks and physical therapy is sometimes recommended. A bandage is placed over the needle insertion site and patients go home shortly after the procedure is completed. There is no widespread long-term data on nucleoplasty. Although there are studies suggesting many patients report relief lasting for at least a year or more after having the transmitter inserted.

Back pain affects anywhere from 80 to 90 percent of the population at one time or another. It’s estimated that nearly 40 percent of the time the source of such discomfort is a herniated disc that’s pressing on nearby nerve roots. Percutaneous disc decompression is proving to be a highly effective method of relief for many patients with pain caused by disc herniation. It’s also a procedure that often eliminates the need for more invasive techniques sometimes requiring accompanying fusion surgery to stabilize the spine.
